A heart problem in a diabetic patient does not always present with pain. Some people expect a loud warning or sudden collapse but medical complications rarely appear this way. They develop gently and gradually. First the arteries become less flexible. Then the heart needs more effort to push blood through stiff walls. Small vessels begin to clog and oxygen supply decreases. The body adjusts and compensates for a long time. One day even a small stress like climbing stairs feels different. An ECG helps find these early changes while they are still reversible.
How Diabetes Damages the Heart Slowly Over Time
The biggest danger in diabetes is not what the patient feels but what the patient does not feel. When glucose remains high it sticks to proteins along artery walls. It behaves like glue. Thickened blood vessels reduce flow and force the heart to pump harder to move blood forward. Over months and years this becomes pressure overload. The heart muscle grows thicker but not necessarily stronger. This is known as hypertrophy. An eletrocardiograma can show early hypertrophy through voltage changes long before symptoms become obvious.
Another factor is nerve damage. The nerves that regulate heart rate and blood pressure can lose sensitivity. A person might not feel chest pain during ischemia which is dangerous because heart tissue may be starving for oxygen without any alarm signal. This silent risk makes Eletrocardiograma and Diabetes a necessary partnership. An ECG does not wait for symptoms. It reads the heart directly.
Early Signs That Suggest ECG Testing is a Wise Decision
Not every diabetic patient experiences clear warning signs. Sometimes the only early clue is slower recovery after activity or a new heaviness after meals. Still there are symptoms worth noticing with serious respect.
- Breathing feels heavier during simple movements
- Fatigue that lingers even after resting
- Heart rhythm that feels irregular or too fast
- Pressure or tightness in the chest
- Ankles or feet swelling by evening
- Sudden dizziness or near fainting
These symptoms do not confirm disease but ignoring them is unsafe. Screening helps build a baseline. Once a baseline exists future ECG comparisons reveal even slight deterioration early. If you want to understand who needs testing sooner you may see the ECG guide.
How an Eletrocardiograma Helps Protect the Heart
An ECG records the electrical impulses that move across the heart muscle. Every beat begins in a conduction node and travels through pathways that allow chambers to contract in rhythm. Diabetes can disturb these pathways. The ECG allows a doctor to observe timing intervals wave shapes and segment patterns. Even small irregular changes might reflect reduced circulation or structural adaptation. This is why early ECG monitoring is more valuable than late detection.
Key benefits for diabetic patients include:
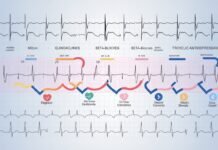
- Identification of early arrhythmias
- Detection of ventricular hypertrophy
- Recognition of ischemic patterns
- Evidence of silent infarction
This information helps doctors adjust treatment. Medication timing dosage exercise recommendations and nutrition planning all rely on accurate heart data. When diabetes and ECG are managed together the patient gains long term protection. Internal cardiac damage becomes visible instead of hidden.
If diabetes is combined with high blood pressure the risk doubles. You may read ECG hypertension for deeper context.
How Often Should a Diabetic Patient Have an ECG
There is no perfect schedule for everyone. Age glucose control family history blood pressure readings and kidney function all influence frequency. Still there are general recommendations used by many physicians.
- One ECG every one to two years for stable diabetic adults
- Annual ECG after age forty or ten years of diabetes
- More frequent testing when symptoms appear
- Mandatory evaluation before major surgery or medication changes
A person with excellent diet control daily exercise routine and good sleep may need testing less often. Another patient with neuropathy or uncontrolled glucose may need testing more regularly. The correct plan should be personal not generic.
How to Prepare for an ECG Without Stress or Confusion
Good preparation improves clarity. ECG does not require fasting or injections. You only need to avoid strong caffeine before testing because stimulants can temporarily raise heart rate. Wear loose clothing so electrodes can be placed quickly. Relax breathing. It is a simple procedure with no discomfort at all. It usually finishes in less than ten minutes.
Some patients worry about results. It is normal to feel uncertain but ECG information is empowering. Knowledge leads to prevention. Prevention leads to protection. The goal is not fear but foresight.
Normal ECG Results Do Not Mean Zero Risk
An ECG reads electrical activity not plaque thickness. Early artery blockages may not show clearly. This is why doctors sometimes recommend further tests such as echocardiogram Holter monitor or treadmill stress evaluation. The best approach uses multiple tools not one single measurement. Diabetes care is like building a wall one brick at a time. ECG is one brick. Diet exercise medication rest and stress balance are the rest.
If you need help interpreting your ECG printout you can review ECG results.
How to Lower Heart Risk With Consistent Habits
There is no miracle cure but there are daily habits that protect the heart with time. Walking improves circulation. Fiber rich foods reduce LDL. Omega three sources lower inflammation. Hydration supports blood consistency. Deep breathing lowers cortisol. Sleep repairs tissue. These habits sound simple because they are. Simplicity is sustainable.
Many doctors also use medication to reduce cardiovascular events. Statins protect arteries. ACE inhibitors support blood pressure control. SGLT2 inhibitors reduce heart failure risk. These are not general rules but personalized strategies built through discussion. The best treatment is the one a patient can maintain with confidence.
For medical prevention guidance see the AHA diabetes resource. If you prefer scientific research findings you may read the NCBI review.
A Human Perspective on Living With Diabetes and Heart Awareness
People with diabetes deserve peace not fear. Awareness is not worry. Awareness is strength. Understanding how ECG and diabetes interact allows someone to take control of their future. Checking the heart is not a sign of weakness but a sign of self respect. It means you want years of healthy living not months of repair. The eletrocardiograma does not replace hope. It supports it.
Conclusion
The heart and blood glucose are connected in ways many people never see. Diabetes quietly shapes the heart from within. ECG reveals those shapes early. By combining Eletrocardiograma and Diabetes management a patient gains safety clarity and years of sustainable health. Prevention is not dramatic. It is gentle and patient. The best day to care for your heart is today.