ECG reading is like interpreting a language. If one letter shifts or one lead loses contact, the message changes in ways that appear meaningful but are not real. Understanding the most repeated errors protects the test value and strengthens clinical decision-making.
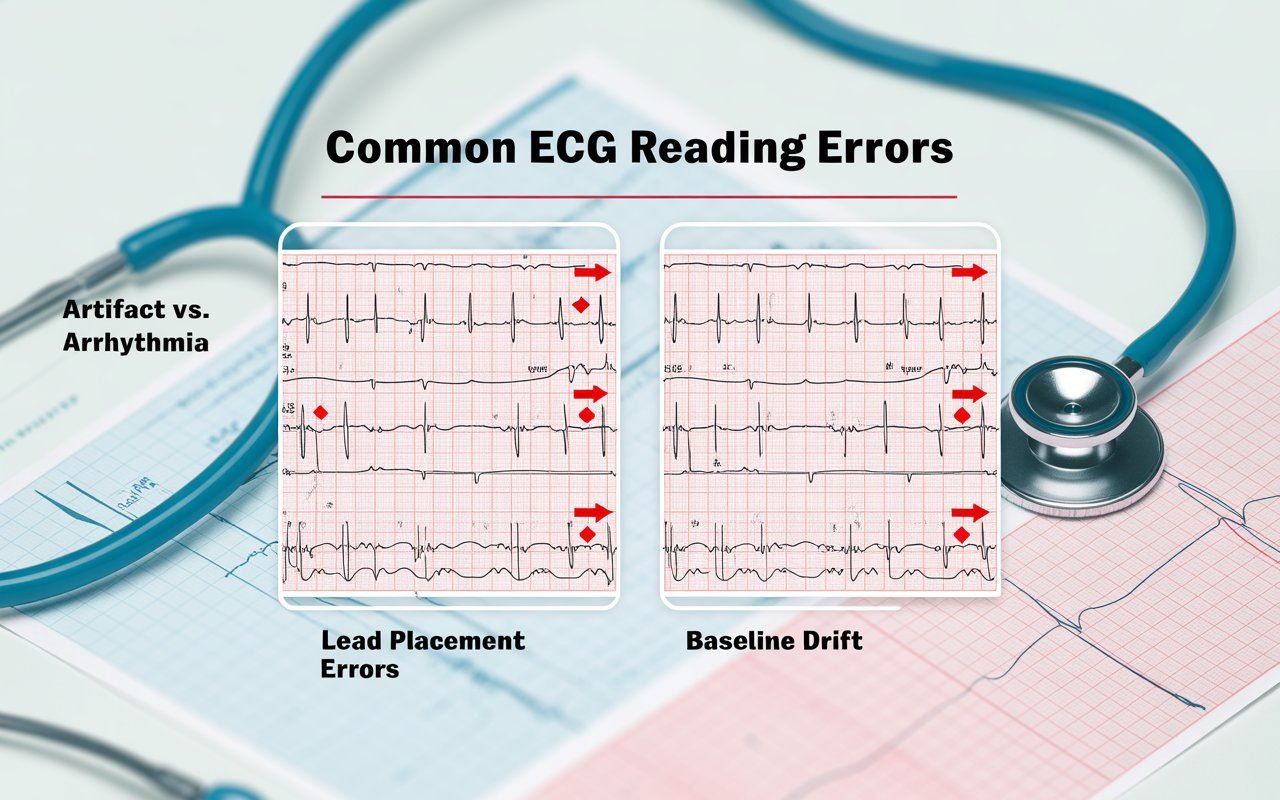
Incorrect Electrode Placement
The most frequent error occurs before the test even begins. If chest electrodes are placed slightly too high or low, the signal direction changes and the ECG wave becomes distorted. This does not reflect true cardiac movement but rather a technical artifact. Small placement shifts may create false ST elevation, T wave changes or bundle branch appearance. Common Eletrocardiograma Mistakes often begin here.
Technicians prevent this by following landmarks, cleaning the skin and confirming placement visually. If you want a clear orientation of position, observe the step by step guide for lead placement reference. Small precision makes large difference.
Muscle Tension and Movement
ECG readings shift when the patient shivers, moves, clenches muscles or talks. Tremor can mimic atrial fibrillation. Jaw movement can create double spikes. Shallow breathing or sudden position change produces baseline drift that looks like ischemia variation. The mistake is not in the heart but in signal interference. Remaining calm, still and relaxed improves accuracy significantly.
Poor Skin Preparation
Oil, lotion and sweat block electrode conduction. When contact weakens, trace becomes noisy or intermittent. This may appear as wandering baseline or chopped QRS patterns. Skin must be dry and electrode gel fully engaged. In athletic or warm-room tests, technicians may wipe chest with alcohol or mild abrasive pad to improve contact strength.
Cold Room Testing
Cold temperature causes muscle tremor. Even slight shiver generates lightning-like interference across the lead pattern. Conducted line appears thick or jagged. Warm comfortable environment prevents this common error.
Misinterpretation of Normal Variants
Some ECG readings look abnormal but reflect normal physiology. Early repolarization pattern appears dramatic in young adults and athletes, yet it is harmless. Sinus respiratory variation can mimic arrhythmia in healthy individuals. The mistake lies in misreading a normal variant as disease. Understanding what is normal prevents false alarm.
For a helpful breakdown of what different waves and intervals mean, refer to results explained which clarifies interpretation well.
Machine Filter Settings
Modern ECG machines use filters to reduce noise. If filters are adjusted incorrectly, real signals may be suppressed or artificial smoothing may appear. High-pass and low-pass settings must match the test purpose. A low filter can remove ST depression, while an improper high filter may exaggerate sharp transitions. Correct configuration reduces misleading wave patterns.
Misreading QT Interval
QT interval is influenced by heart rate, medication, and electrolyte balance. If corrected QT (QTc) is not calculated properly, results may appear abnormal even when safe. This is one of the most Common Eletrocardiograma Mistakes in clinical review. Slow heart rate can make QT look longer than it truly is. Fast heart rate shortens it falsely. QTc correction formula prevents this mistake.
Ignoring Medication Influence
Some drugs naturally prolong or shorten conduction. Antiarrhythmics, antidepressants, diuretics and certain antibiotics can alter QT or PR intervals. If medication history is unknown, tracing may appear alarming when it is simply treatment effect. A good reading always matches rhythm to clinical context.
A detailed breakdown of medication influence is available in Article 26 at ECG meds.
Not Allowing Rest Before Test
ECG should not be performed immediately after rush, exercise or emotional agitation unless stress evaluation is intended. Heart rate remains elevated and sympathetic tone affects conduction automatically. This may produce false tachycardia or ST drift. Waiting several minutes stabilizes rhythm.
Noise Interference
Nearby electronics, phone vibrations, loose wires or power sources may create alternating current interference. The pattern resembles tremor wave and confuses reading. Turning off devices or relocating cables improves clarity.
Hyperventilation Error
Deep fast breathing before ECG sometimes lowers carbon dioxide, shifts pH and widens ST appearance. This can be mistaken for ischemia. Calm natural breathing avoids misinterpretation.
Rushing Through Interpretation
Some errors occur not during testing but afterward when reading is rapid or incomplete. A careful review checks rate, rhythm, axis, intervals, wave morphology, ST patterns, and progression across leads. Each element contributes to meaning. Slow interpretation is safer interpretation.
How to Avoid Common Eletrocardiograma Mistakes
Accuracy begins with preparation. Clean skin, correct electrode placement, relaxed posture and stable filters produce trustworthy recordings. After that comes interpretation. Clinicians compare waves with symptoms, medication history, electrolyte status and previous ECGs when available. Combining technical precision with clinical judgment reduces nearly all avoidable errors.
Mayo Clinic also provides open heart health education at mayo clinic, which helps general readers understand rhythm and testing basics. Cardiovascular awareness resources for public health are also available through American Heart Association at heart org for broad patient education.
Final Summary
Wrong ECG readings occur when preparation is rushed, interpretation is incomplete or electrode contact is weak. Most issues do not come from the heart but from process. Recognizing Common Eletrocardiograma Mistakes protects test accuracy and reduces unnecessary concern. Care, patience and correct technique transform the ECG from complicated lines to a reliable map of heart function.